Ear infections can be a common issue for many people, and if you’re a hearing aid user, you might be wondering if you’re more susceptible. While wearing hearing aids doesn’t directly cause ear infections, it can increase your risk. No need to worry, though! With the right knowledge and care, you can keep your ears healthy and enjoy the full benefits of your devices.
In This Article:
Can Hearing Aids Cause Ear Infections?
Hearing aids themselves do not directly cause ear infections, but they can contribute to the risk if not properly managed. Ear infections can happen when bacteria or moisture are trapped in the ear canal, and there are a variety of factors that can make this more likely, even with proper cleaning practices.
One common reason is the buildup of moisture in the ear. Hearing aids, particularly in-the-ear styles, can trap moisture in the canal because of sweating, humid weather, or even naturally occurring earwax. Moisture creates an ideal environment for bacteria to grow, increasing the risk of an infection.
Additionally, ill-fitting hearing aids can lead to irritation or pressure sores. If the skin in the ear canal is irritated or broken, bacteria can easily enter and cause an infection.
Regular cleaning can help, but even then, an infection can still occur. As a preventive step, it’s good to take the hearing aid out from time to time, letting your ear ‘breathe’ whenever possible. Try to also keep your ears dry and avoid wearing the aids if you feel any discomfort. If in doubt, a check-up with your audiologist or hearing care provider can help address fit or moisture issues and keep your ears healthy.
Types of Ear Infections
Ear infections can affect different parts of the ear, each with unique causes and symptoms. Understanding these infections can help you identify and manage them effectively.
(1) Middle Ear Infections (Otitis Media)
Middle ear infections, also known as otitis media, occur in the air-filled space behind the eardrum where small bones of the ear (ossicles) are located. This type of infection is often caused by fluid being trapped behind the eardrum, typically due to colds, allergies, sinus infections, or other issues that can cause congestion.
- Causes: Colds or flu, allergies, blocked Eustachian tubes
- Symptoms: Ear pain/ feeling of pressure, muffled hearing, fluid drainage, fever
A middle ear infection can make it challenging to use hearing aids due to discomfort or a feeling of fullness in the ear. The buildup of fluid can also affect how sound travels to the eardrum, making everything sound muffled. If you suspect a middle ear infection, it’s best to remove your hearing aids until the infection subsides and consult your doctor for treatment.
(2) Outer Ear Infections (Otitis Externa/Swimmer’s Ear)
An outer ear infection, also called Otitis Externa or ‘swimmer’s ear,’ affects the ear canal from the entrance up to the eardrum. This infection is often the result of water getting trapped in the ear after swimming, creating an environment where bacteria can thrive. It can also occur if the ear canal becomes scratched or irritated, allowing bacteria to enter.
- Causes: Water trapped in the ear canal, excessive cleaning or use of objects in the ear, allergic reactions to earplugs or hearing aid materials
- Symptoms: Pain or tenderness, ear tenderness to touch, redness and swelling of the ear canal, itchiness, fluid discharge
Outer ear infections can make wearing hearing aids painful due to swelling or irritation in the ear canal. In some cases, it may also cause your hearing to go muffled. If you have any pain, make sure to leave the hearing aids out and allow your ears to heal. Wearing them while suffering from an infection might make the condition worse or prolong it, so before inserting the aids back in your ears, make sure to see your hearing care provider and follow their advice.

How Can I Avoid Ear Infections While Wearing Hearing Aids?
The best way to prevent ear infections when wearing hearing aids is to prevent the circumstances that cause the infections in the first place (duh, right?). As already mentioned, the main culprits are usually moisture, bacteria, and irritation, so you need to learn to avoid those. Have a look below for some helpful habits:
(1) Keep Your Ears Dry
Moisture can create the perfect environment for bacteria to grow, increasing the likelihood of infections. It’s important to keep both your ears and your hearing aids dry.
- Avoiding Moisture Buildup: Always remove your hearing aids before bathing, swimming, or engaging in activities that may cause excessive sweating. This will help prevent water from getting trapped in the ear canal or hearing aid.
- Use of Hearing Aid Dehumidifiers: Consider using a hearing aid dehumidifier to remove any moisture that may have accumulated during the day. Dehumidifiers come in two forms: simple desiccant jars that absorb moisture, or more advanced ‘dry & store’ systems that use gentle heat and UV light to sanitise your hearing aids.
(2) Ensure Proper Fit
As time goes by, our bodies change, including our ears. Even if your hearing aid was a perfect fit for you when you first purchased it, this might not be the case any longer.
If your hearing aids are uncomfortable, they could be pressing against the skin or causing friction, irritating the ear canal, and creating small scratches, which can lead to infection. On the other hand, hearing aids that are too loose can allow moisture or debris to enter the ear canal.
In case you’re experiencing any discomfort, make sure to visit your audiologist for an adjustment.
(3) Clean Your Hearing Aids Properly
As we’ve pointed out, wax and bacteria can easily accumulate on your aids, which can increase the risk of infections if not cleaned regularly.
- Tools and Techniques: Make sure you have some tools on hand, such as a wax pick or a soft brush, to remove earwax and debris from the openings of your hearing aids. Remember to replace the wax guards as needed.
- Daily Cleaning Routine: Get into the habit of cleaning your hearing aids every day, ideally before bedtime. This allows them to ‘breathe’ overnight and ensures no moisture or debris remains when they are not in use.

What Do I Do if I Wear a Hearing Aid and Get an Infection?
If you develop an ear infection while using hearing aids, don’t panic. Instead, take some precautions to prevent the infection from worsening, and to make sure your ears heal properly:
(1) Steps to Take Immediately
- Remove Your Hearing Aids: Take out your hearing aids as soon as you notice any signs of an ear infection, such as pain, swelling, or discharge. Removing your aids gives your ear a chance to ‘breathe’ and helps reduce the buildup of bacteria and moisture that can aggravate the infection.
- Keep Your Ears Dry: Moisture can make an ear infection worse, so it’s important to keep your ears as dry as possible. Avoid swimming or getting water in your ears when showering. You may also use a clean, soft towel to pat your outer ear dry.
- Clean Your Hearing Aids: Be sure to clean your hearing aids thoroughly to remove any bacteria that may have caused or contributed to the infection. This will help prevent reinfection once your ears have healed. Replace wax guards and clean all surfaces with the appropriate tools.
(2) When to Seek Medical Help
If you notice any discharge, the symptoms of your ear infection do not improve after a couple of days, or the pain becomes more intense, seek medical advice from your healthcare provider or GP. You may need antibiotics, or ear drops to clear the infection and reduce inflammation.
(3) Using Your Hearing Aids During an Ear Infection?
- Limit Use: If you need to wear your hearing aids during an ear infection, limit their use to essential times only. Wearing them for longer periods may worsen irritation.
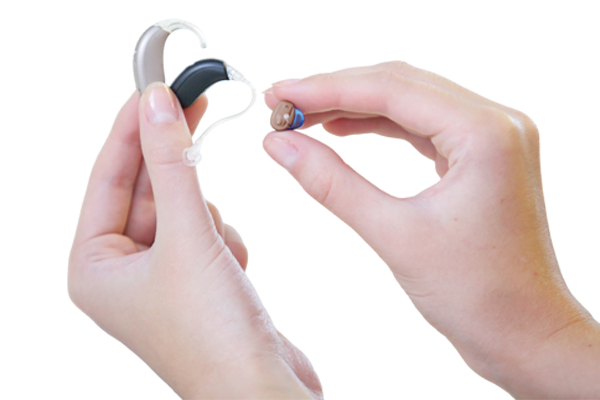
- Use Open-Fit Hearing Aids: If you have both in-the-ear (ITE) and behind-the-ear (BTE) hearing aids, consider using the BTE ones during the infection. They typically allow for better airflow and are less irritating to the ear canal.
- Keep Everything Clean: If your doctor allows you to continue wearing your hearing aids, it is crucial to clean them daily to prevent the spread of bacteria. Make sure to sanitise the earmould or dome, and replace any wax guards.
(4) Follow-Up With Your Hearing Care Professional
Once your infection has cleared up, make sure to schedule a follow-up appointment with your audiologist. They can check that your hearing aids fit correctly and make any necessary adjustments to prevent future irritation.
It can also be a good idea to have your aids professionally cleaned to make sure they are free of any residual bacteria.

FAQ
Can you wear a hearing aid with an ear infection?
Wearing a hearing aid with an ear infection is generally not advised, letting your ears breathe and heal without any friction or irritation can speed up the recovery process. However, if you do need to wear them for short periods of time, make sure they are clean and dry. Always consult your doctor for advice based on your specific condition.
Can wearing hearing aids cause ear infections?
Wearing hearing aids doesn’t directly cause ear infections, but improper use can increase the risk. Hearing aids and ear infections are often linked due to factors like moisture, bacteria buildup, or an ill-fitting device that irritates the ear canal. To reduce the risk, make sure to maintain good hygiene by cleaning your hearing aids regularly and ensuring a proper fit.
What can I use to treat an ear infection as a hearing aid wearer?
If you have an ear infection while using hearing aids, your doctor may prescribe ear drops suitable for hearing aid wearers to help treat it. Remember to always remove your hearing aids before applying ear drops, and wait for your ears to dry completely before putting them back in. If you’re unsure or have any concerns, it’s best to consult your audiologist.
Can ear drops damage hearing aids?
Yes, ear drops can damage your hearing aids if they come into contact with them. Make sure to remove your hearing aids before applying ear drops and wait until the drops are fully absorbed before reinserting your aids. Make sure to always follow your GP’s instructions.
Is my ear infection from hearing aids?
If you suspect your ear infection might be due to wearing hearing aids, consider any recent discomfort or irritation you may have experienced. That could have been due to a poor fit. Lack of a good hearing aid cleaning routine could also be the culprit behind your ear infection. If any of those factors apply to your situation, your ear infection could be related to your hearing aids.
Can an ear infection cause hearing loss?
Yes, it is possible to experience hearing loss from an ear infection. Middle ear infections can cause fluid buildup behind the eardrum, leading to temporary hearing impairment. If untreated, repeated or severe ear infections can result in more lasting damage to the structures of the ear, potentially leading to permanent hearing loss. It’s important to seek medical attention if you suspect an ear infection to prevent any long-term impact on your hearing.
Need Help with Your Hearing Care?
If you’re experiencing any symptoms of an ear infection or need an adjustment to your hearing aid fit, or even a professional cleaning, get in touch with us at Hear4U – we’re here to take care of all your hearing needs!






